


















Joe Schiel (1956-2016)
I am starting a non-profit organization called Butterflies for Joe. There are two reasons we chose this name. One is very personal and spiritual to us. The other is a reference to the “Butterfly Effect,” which is the concept that states small causes can have larger results — a butterfly flapping its wings over the ocean in India can produce a ripple effect which can cause a tsunami on the other side of the world. This is our plan for Butterflies for Joe. I believe real change will happen when families are having conversations about drugs. When doctors are aware of akathisia and have honest and informed conversations with patients. I am not anti-drug. I owe my livelihood to the hard work my husband did in the pharmaceutical industry for 37 years. But, antidepressants that alter the mind, shouldn’t be given to someone at the onset of situational stress. It is not a medicine for someone that doesn’t have chronic issues. It is a medicine that deserves to be used by those that truly need it.
OUR STORY
There is nothing like true love — either between adults or with your children. I would say my story has just to do with my husband, but losing your loved one in such a tragic way is a whole family issue. Any death is. But the way we lost Joe was horrific. And it didn’t have to happen.
My guy, my partner, my best friend, the person I couldn’t wait to talk to every day, my laughing buddy, who was a mentor, successful, fun, ornery and the love of my life was killed by an antidepressant (SSRI – Selective Serotonin Reuptake Inhibitor) given for short term stress he was experiencing.
In early 2016, Joe’s work situation changed and added additional stress to his life. But he knew it was short term stress. He was in the pharmaceutical sales business for over 37 years. He was a regional manager whose territory was half the country. Due to a series of people being let go and his boss’s retirement, Joe’s workload had more than doubled for the time being. But Joe understood that this was temporary and he was not overly stressed about it. He even had a physical on April 19th, and in the doctor’s notes from that check-in he told her that he had additional stress but it was not anything he could not handle.
This was 3 weeks before he started on the generic version of Lexapro.
Shortly after April 19th, we decided it was time for Joe to retire and he was planning on giving his notice on July 8th . We were so excited! Shortly after we made this decision – and still 3 weeks before starting Lexapro – we found our perfect retirement home in the Lake of the Ozarks! It was also on the lake and a golf course and was perfect! We were like kids in a candy shop as we started imagining our retired life together.
But the reality of buying and selling homes on top of the workload was, I believe, what made him call his doctor.
On May 10th, Joe called his internal medicine doctor and asked for Lexapro — or something to help him get through the additional stress. She immediately called in the prescription for the generic version of Lexapro, which is escitalopram, without talking with him in person and sharing the possible side effects with him. FDA guidelines state that this medication should not be prescribed until a patient has had 6 consecutive documented months in a row of expressing general anxiety. Would an in-person conversation with Joe’s doctor have made a difference? Probably not because she most likely wasn’t a where of the additional risk on suicide in people over 24.
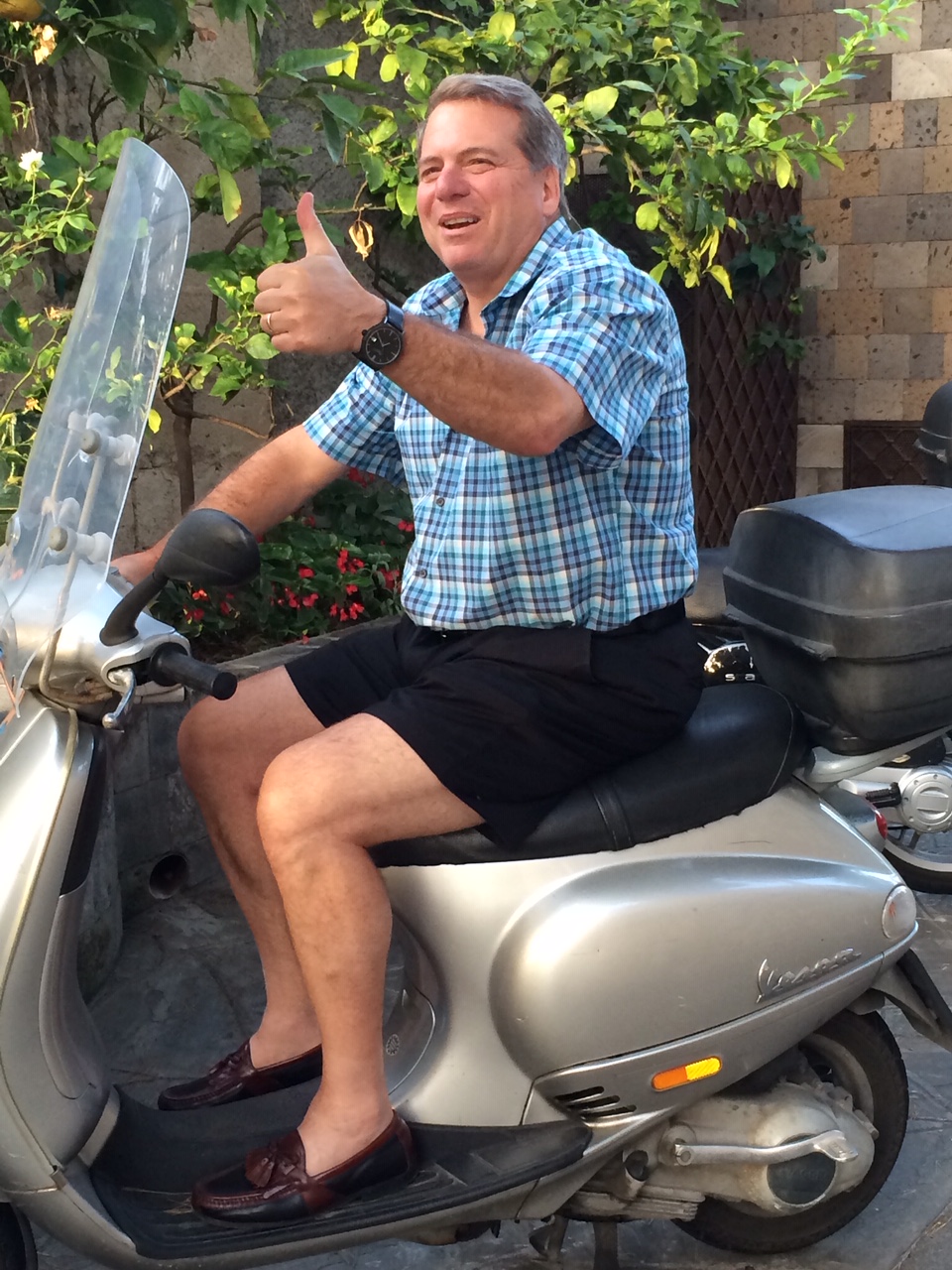
I knew something was wrong but I just associated it with the overall situation. But as time went on, I could tell it was more. He had become agitated, paranoid, restless and wasn’t sleeping. We were leaving on an anniversary trip and were going to Italy for 5 days and then to Croatia for a company awards trip where he was getting an award for Region Manager of the year.
By this time, June 3rd, Joe’s overall demeanor had completely changed. He wanted to cancel the trip, which is completely not in character with my husband. We loved to travel and were so excited about our plans. He loved awards trips! But he was acting so crazy. I looked at him and asked him what he was taking. In 30 years of marriage I never confronted him about his medications — he was always the family “doctor.” Because of his familiarity with the pharmaceutical industry, when any of us were sick, he would tell us what we needed and then we told our doctors. They always gave us what he said. So I never questioned any of his prescriptions.
When I finally confronted him, Joe looked at me with his arms crossed over his chest and said he was on Lexapro. It was like a light bulb turning on in my head. In 2009, his company was bought out and he needed to find a new job. Well, with a family of four, a big house and limited time on his company’s insurance, he was stressed. He asked the doctor for something to get him through and she put him on Lexapro. I didn’t know it then, but at one point I thought he was having a nervous breakdown. I begged him to go to the hospital and he agreed. We went to a psychiatric hospital but he wouldn’t go in. He said to take him home and he would get off all the meds. I didn’t understand what he meant by that but assumed, again, that he knew what he was doing. And he did get better once he went off Lexapro.
Once the light bulb went on days before our big Italy and Croatia trip, I begged him to wean off the drugs. I told him it was making him crazy. He told me he would but I don’t know if he did. He may have tried and then taken more. I didn’t watch him take them. I trusted him to wean off them. But I didn’t realize what was happening to his body was beyond his control. I didn’t know how bad withdrawal could be either.
We left for Europe and I thought this trip would do him good by being away from work and dealing with our real estate ventures. But I was so wrong.
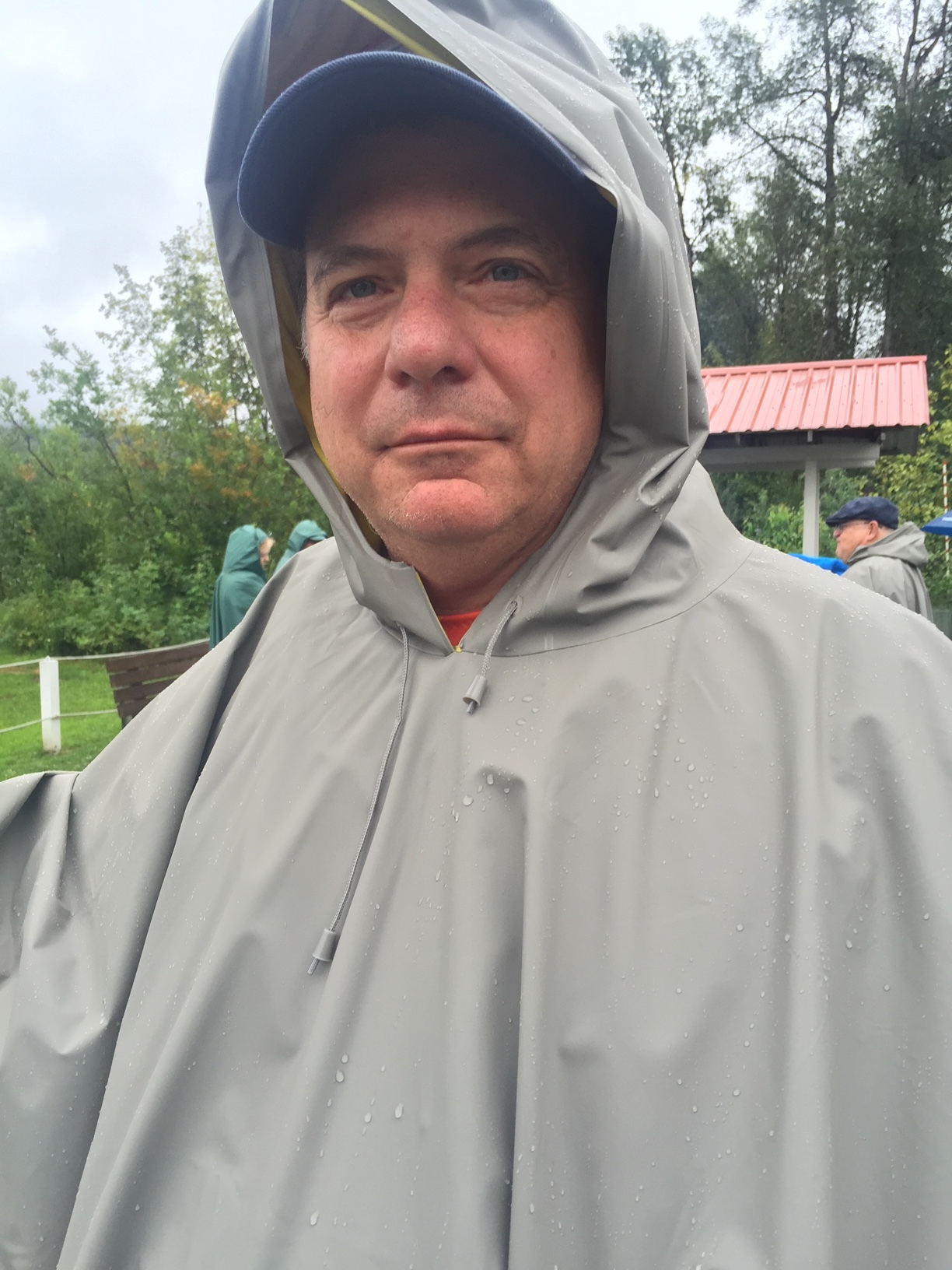
In Italy he became obsessed with crazy things — doing things that weren’t in his character, like not being able to carry a conversation with anyone. He wasn’t sleeping and when he did, he had horrible dreams. By the time we reached Croatia, he was a mess. We were on the way to the opening event for the awards trip and he begged me to get him out of there. I just kept thinking I could get him home and it would be all right. The thoughts in his mind were so bad but he wouldn’t tell me. He just was even more paranoid and restless — all signs which I know indicate he was suffering from akathisia. His friends didn’t know what was wrong with him. I kept telling everyone that he had the stomach flu. He couldn’t talk with any of them. By this time he thought they were listening in our room and the group photographer was spying on us. He thought they were trying to prove that he didn’t have the flu, showing just how intense his paranoia had become.
I finally had to tell someone. Right before the big awards dinner he told me he thought was having a heart attack. I didn’t think he was but that is what he told me. I ran out of the room to one of the guys Joe worked with who was also on the trip. He was with his wife, who is a doctor, and a travel director. I told them he was having a bad reaction to Lexapro and I didn’t know what to do. I was crying at this point and I was so scared. When we went back to our room, he was standing outside and looked fine. I was so puzzled. He and his friend hugged and we went to the dinner. But the paranoia continued through the dinner.
His friends asked us to go to the bar when we got back. I didn’t want to go, but we did. He stood at the bar and didn’t drink or talk but he smiled at everyone. I remember thinking how handsome he looked. When we finally left the bar, he simply said to me “it is all over.” I asked him why he said that and he couldn’t give me any more of a response. I reminded him of how great the night went and how many people loved him! He didn’t say anything else. When we got back to our room, he got in bed and completely covered his head. That was odd but I thought maybe he was relieved to have gotten through that night and was finally going to sleep. It had been so long since he had any good sleep.
The last thing he said was to not forget to set the alarm for our tour the next day.
About 10 minutes later he got out of bed and was pacing. He then starting putting on his shorts and I asked where he was going. He hadn’t been out of my sight the whole time. He just said, “I am going to jump.” I can’t even put into words the panic I felt. I jumped out of bed and said you are not and I tried to grab the phone. He wouldn’t let me and we struggled while I screamed for help. He was so strong. Somehow I was able to turn him around and I slapped him twice across the face, trying my hardest to bring him out of this possessed state of mind he was in. He was sitting on the bed then and when he looked at me, I swear his blue eyes were gone. His eyes were all white. My sweet husband was already gone. Somehow in an instant he flew passed me and onto the balcony. I tried desperately to stop him from jumping but I couldn’t.
WHAT HAPPENS NEXT?
It is not an easy story to tell; much less hear. I share it because I want others to learn how horrific the wrong medication can be. There are many people I have met who are working to raise awareness and end medication-induced suicide and violence. But they need to be heard by everyone. Everyone needs to know the potential harm that can come to him or her or someone they love.
Pharmaceutical companies do not make our general doctors aware of the growing numbers of people older than 25 having suicidal ideation or having violent actions. But the facts speak for themselves. Pharmaceutical companies are able to argue that they do inform patients of these side effects, but they are buried in the tiny print that comes along with any prescription medication — think about all of the pharmaceutical commercials you hear on TV with someone speaking so fast you can barely understand them. The problem is, these deadly and very real side effects are not emphasised by doctors or pharmacists — and most importantly, everyday people like Joe and myself didn’t even know this was something to look out for. But attention needs to be paid to this and most doctors I have spoken to don’t even know about this problem. One doctor even laughed at me when I said they need to monitor their patients on these medications sooner than 30 days. It was even suggested by the FDA that children be monitored weekly. She casually just told me, “like that is ever going to happen.”
We need to keep fighting and making awareness of what can happen. We need to educate our doctors on what the pharmaceutical companies are not. When I told my internist what happened she was horrified. She told me she gives out these medicines like she gives out Halloween candy. She had no idea that over 325 million people in our country alone are on SSRI’s, much less the horrific results for between 5 – 8% (depending on the drug) of patients who kill themselves or someone else while suffering from akathisia.
